
Dermal fillers have become an essential tool in aesthetic medicine, offering patients a non-surgical way to enhance their facial features. However, while generally safe when administered correctly, complications can arise. One of the most serious complications is vascular occlusion, which occurs when a filler blocks a blood vessel, leading to restricted blood flow.
Recognizing the signs of vascular occlusion after filler early can prevent severe consequences such as tissue necrosis or even blindness. This article provides a comprehensive guide for medical aestheticians on how to recognize, respond to, and prevent vascular occlusion to ensure patient safety.
What is Vascular Occlusion?
Vascular occlusion occurs when a blood vessel becomes blocked, preventing blood from flowing properly to surrounding tissues. In the context of dermal fillers, this can happen when the filler is injected directly into a vessel or compresses a nearby artery or vein. Without timely intervention, this blockage can lead to tissue ischemia (restricted oxygen supply) and, eventually, necrosis (tissue death).
How Does Vascular Occlusion Happen During Filler Injections?
There are two primary ways vascular occlusion can occur:
- Intravascular Embolism – The filler is injected directly into an artery, blocking blood flow and preventing oxygen from reaching downstream tissues.
- Extravascular Compression – The filler is placed near a blood vessel and exerts pressure, reducing or completely blocking circulation.
Both scenarios can lead to serious complications, including severe pain, skin discoloration, and tissue death. In extreme cases, if an artery supplying the eye is affected, it can result in vision loss or blindness. To learn more about lip filler vascular occlusion read our article.
Early Signs of Vascular Occlusion
The ability to recognize early warning signs is critical for medical aestheticians. Prompt intervention can mean the difference between full recovery and permanent tissue damage.
Immediate Signs (Within Minutes to Hours)
- Sudden, Severe Pain During Injection – A sharp, intense pain that is more severe than usual injection discomfort.
- Blanching (Skin Whitening) – The affected area may turn pale or white due to restricted blood flow.
- Delayed Capillary Refill – When pressed, the skin does not regain its normal colour within two seconds.
- Cold Skin Temperature – The affected area feels cooler to the touch compared to the surrounding skin.

Progressive Signs (Hours to Days)
If left untreated, vascular occlusion symptoms will worsen:
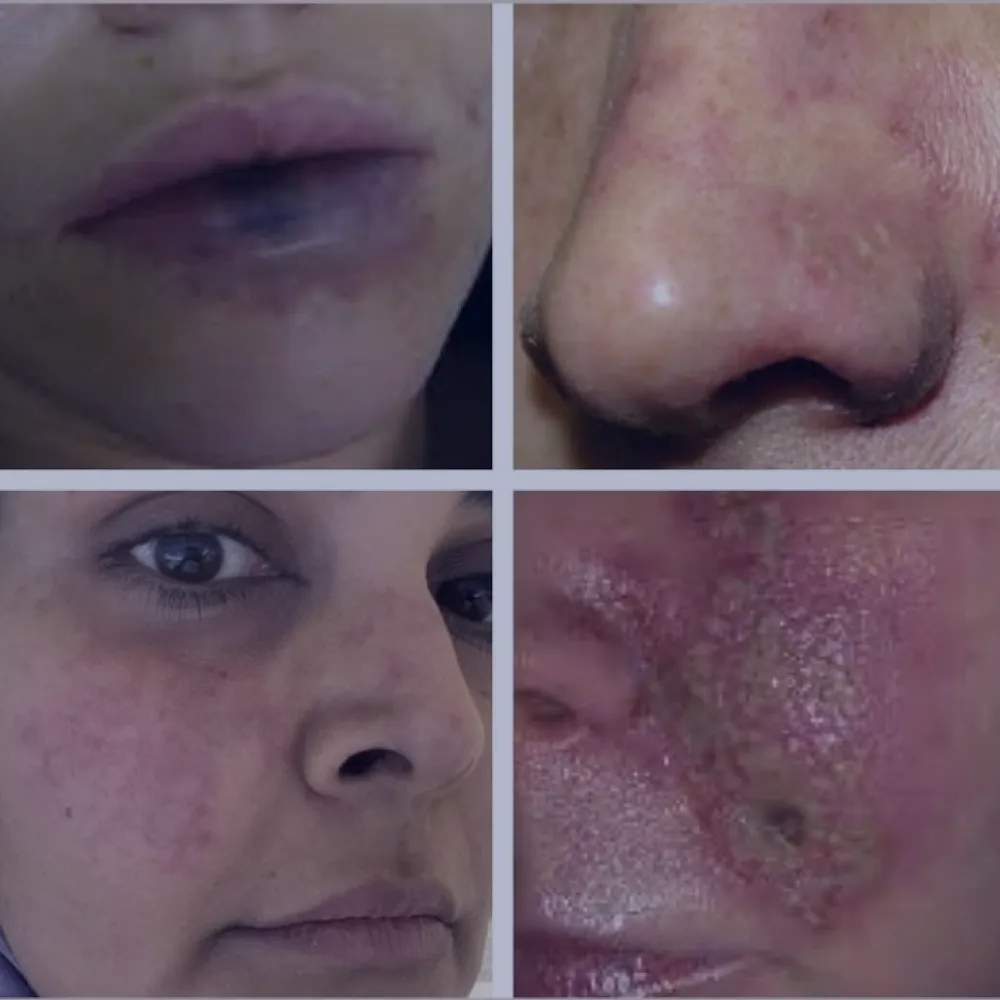
- Livedo Reticularis (Mottled Skin Appearance) – A lace-like, purplish discoloration of the skin, indicating worsening blood flow restriction.
- Persistent, Worsening Pain – Pain that intensifies over time, often described as throbbing or aching.
- Development of Purple or Blue Bruising – While normal bruising from filler fades over time, vascular occlusion-related bruising may darken or spread.
- Skin Breakdown and Ulceration – If the blockage is not resolved, skin tissue may start to break down, forming open sores.
Vascular Occlusion vs. Bruising: How to Tell the Difference
Post-filler bruising is common, but differentiating between a normal bruise and vascular occlusion is crucial:
Key takeaway: If a patient exhibits delayed capillary refill, persistent pain, or blanching, vascular occlusion should be suspected and treated immediately.
Immediate Actions if Vascular Occlusion is Suspected
If vascular occlusion is suspected during or after a filler procedure, immediate intervention is critical to prevent severe complications, including tissue necrosis or blindness. Follow these essential steps:
- Stop the Injection Immediately – Cease any further filler administration as soon as vascular occlusion is suspected. Continuing to inject can worsen the blockage and increase the risk of tissue damage.
- Assess Capillary Refill – Press the affected area with light pressure and release. If the skin does not regain its normal colour within 2 seconds, blood flow is likely compromised, indicating vascular occlusion.
- Massage and Apply a Warm Compress – A gentle but firm massage can help disperse the filler and improve circulation. Apply a warm compress (not hot) to the area to encourage vasodilation and improve blood flow.
- Administer Hyaluronidase (If Using Hyaluronic Acid Fillers) – Injecting hyaluronidase quickly can dissolve the filler and restore circulation. Use higher doses if necessary, depending on the severity of the occlusion.
- Provide Aspirin (If No Contraindications) – A low dose of aspirin (75-100mg) may help prevent clot formation and promote circulation. However, ensure the patient has no contraindications to aspirin use.
- Consult a Specialist Immediately – If symptoms persist or worsen despite intervention, refer the patient to a vascular specialist or emergency care immediately. Cases involving eye involvement require urgent medical attention to prevent vision loss.

Prevention Strategies for Practitioners
Ensuring patient safety during filler injections requires more than just technical skill—it demands a proactive approach to prevent complications like vascular occlusion. By adopting best practices in injection techniques, understanding facial anatomy, and staying prepared for emergencies, practitioners can significantly reduce risks. Here are key prevention strategies every aesthetic injector should follow.
1. Understand Facial Anatomy
- Avoid high-risk areas in the glabella, nose, and lips, which have complex vascular structures.
- Use ultrasound guidance for safer injections when available.
2. Use Safe Injection Techniques
- Aspirate Before Injection – Pull back on the syringe before injecting to check for blood.
- Use a Cannula Instead of a Needle – Cannulas are less likely to penetrate blood vessels.
- Inject Slowly and in Small Amounts – Avoid excessive pressure and large filler boluses.
3. Monitor the Patient Closely
- Observe for any immediate adverse reactions.
- Educate patients on post-treatment warning signs.
4. Have an Emergency Kit Ready
- Always have hyaluronidase, aspirin, nitroglycerin paste, and warm compresses on hand.
- Train staff in emergency protocols for vascular occlusion management.
Long-Term Effects and Patient Recovery
Even when treated promptly, vascular occlusion can have lasting effects. Proper post-care is essential to ensure full recovery and prevent complications.
- Monitoring for Delayed Symptoms: Some vascular occlusions may not become fully apparent until 24-48 hours post-treatment. Patients should be instructed to report any worsening pain or color changes.
- Post-Treatment Skin Care: Encouraging gentle massage, warm compresses, and avoiding strenuous activity can support healing.
- Follow-up Appointments: Patients should return for evaluation within 48-72 hours to assess tissue recovery and identify any lingering issues.
Proper post-care education ensures patients recover safely and maintains their confidence in the practitioner.
Conclusion
Vascular occlusion is a serious but preventable and treatable complication of dermal filler injections. Early recognition of signs, combined with quick and appropriate intervention, can prevent irreversible tissue damage.
Medical aestheticians should stay informed about vascular occlusion protocols and participate in specialized training, such as the Aesthetic Complications Course , and also attend Facial Anatomy Course to enhance patient safety and professional expertise.
References
- Dr Tim Pearce – 5 Early Warning Signs of a Vascular Occlusion When Injecting Fillers
- Harley Academy – Bruising or Vascular Occlusion: How to Tell?
- Phi College – Recognising Vascular Occlusion in Dermal Filler Treatments
https://www.phicollege.com/dermal-fillers-course/recognising-vascular-occlusion/
Disclaimer:
This article is intended for licensed medical professionals. All protocols, dosages, and treatment insights referenced herein are based on published literature. The content is not intended to encourage application, diagnosis, or self-treatment of unlicensed individuals, and should not be used as a substitute for the clinical judgment of a qualified healthcare provider.
